Student Profiles: NIH Funding Advances Health Sciences and Trains Biomedical Leaders at Georgetown University Medical Center
As an R1 research institution, Georgetown University is dedicated to fostering discoveries and scientific advancements while training the next generation of researchers. Research and training at Georgetown University Medical Center (GUMC) thrive thanks in part to significant support from the National Institutes of Health (NIH).
Historically, Georgetown and the NIH have worked together to produce monumental breakthroughs in human health, such as discoveries leading to the development of the HPV vaccine – the world’s first cancer prevention vaccine. Today, in April 2025, GUMC researchers are named in over $66 million of active NIH awards furthering the work of more than 150 principal investigators in areas ranging from aging and Alzheimer’s disease, to cancer treatment, to neuroscience and pharmacology, to mental health.
Of that NIH funding, nearly $3.8 million comes through T32 and TL1 training grants, which may fund tuition and stipends, conference travel, biostatistics consultation, and other resources that facilitate research and training – giving students and postdoctoral fellows the opportunity to learn from leaders in biomedicine while contributing to cutting-edge, impact-focused projects.
“We’re proud of our success at GUMC in securing NIH funding for research and training programs,” said Anna Riegel, the medical center’s vice president for biomedical education and research. “It’s a testament to the dedication of our faculty, postdocs and students, and to Georgetown’s impact in advancing biomedical science.”
GUMC hosts nine T32 Institutional Training Grants, as well as one TL1 Linked Training Award program. More than 170 doctoral students and 60 postdoctoral associates have participated in these programs, with many going on to take positions as research staff, faculty, postdocs, and professionals in science policy and biotech.
“Our NIH-funded T32 programs at Georgetown provide incredible training opportunities for our Ph.D. students and postdocs, with impacts stretching beyond those who are directly funded by these programs,” said Elizabeth Salm, director of graduate and postdoctoral training and development for Georgetown University Biomedical Graduate Education (BGE). “Students and postdocs in the programs have explored their career interests and built their research skills individually using T32 funding through internships and external training, which has led to some alumni finding roles in tech transfer, science policy, and project management.”
BGE spoke with four current NIH grant-supported Ph.D. students about their research, their studies, and how their programs are helping them reach their career goals. These students are all working to address critical health challenges – including neurodegenerative diseases, cancer progression, and pregnancy complications – in hopes of building the path to a healthier future. Amid changes in federal funding that cast uncertainty on biomedical research, their motivation serves as inspiration to continue overcoming challenges and pursuing advancements in the health sciences as “people for others.”
Briana Bernstein: Understanding Neurological Disorders

Briana Bernstein
For Briana Bernstein, joining the Interdisciplinary Program in Neuroscience (IPN) was an opportunity to deepen her understanding of brain circuitry and neurological disorders such as Parkinson’s disease and epilepsy.
As a third-year Ph.D. student, Bernstein works under the mentorship of Rebekah Evans and Patrick Forcelli, bridging the gap between neuroscience and pharmacology. She is currently conducting research on two brain structures that are vital for sensorimotor integration: the superior colliculus, located in the midbrain and responsible for visually guided actions, and the pedunculopontine nucleus (PPN), important for movement, posture, gait, and arousal. In doing so, Bernstein hopes to uncover how these regions might be related to neurological disorders.
These disorders “[are] one of those things I’ve always been interested in,” Bernstein said. “This brain circuit is implicated in Parkinson’s as well as epilepsy, so we think we can target the extended basal ganglia circuit. [The superior colliculus and PPN] aren’t part of your traditional basal ganglia circuit, but there’s a lot of interconnectivity there.”
In order to parse out these brain regions, Bernstein has been looking at neurological function in healthy mice. She uses techniques such as viral neuronal tracing, in which a viral vector that responds to light is injected into mice for electrophysiology experiments. Once axons in the superior colliculus are stimulated, she can record neuron activity in the PPN and examine how it interacts with the superior colliculus – and why.
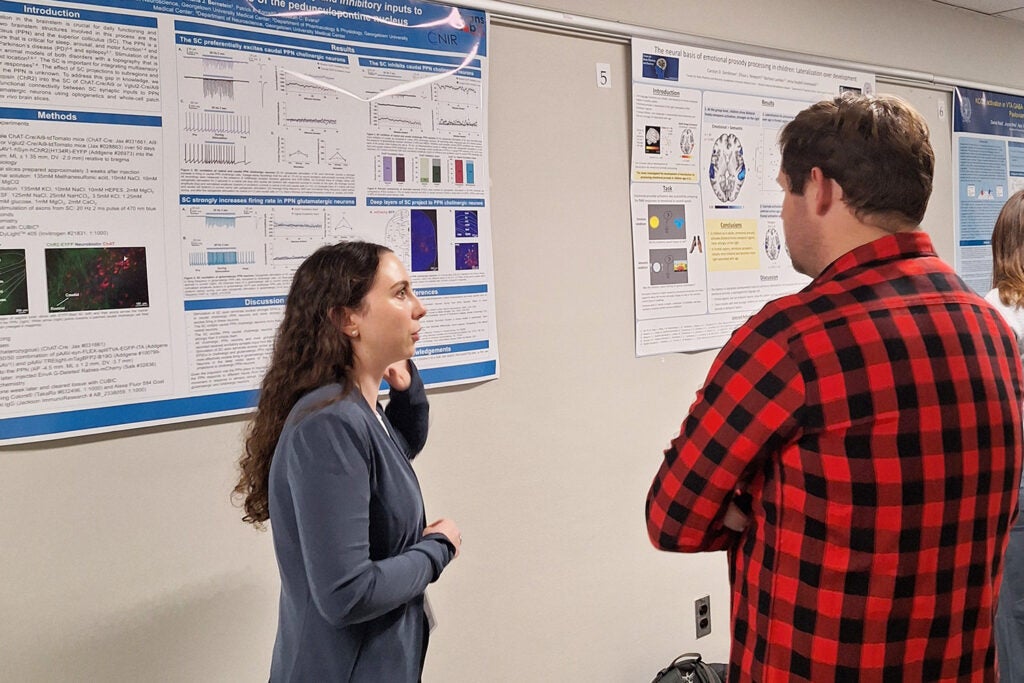
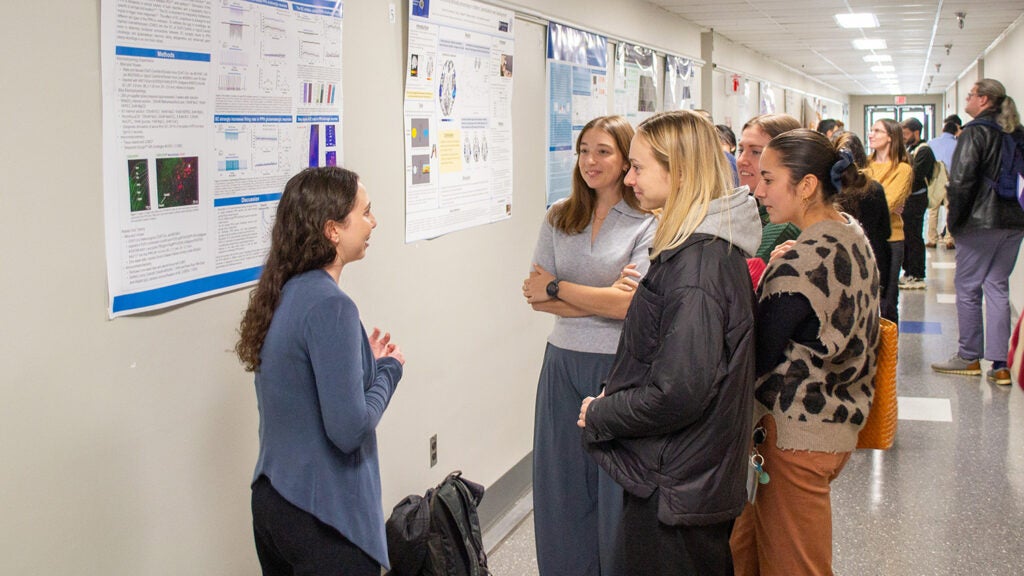
Bernstein presents her work at Student Research Day in 2024.
Bernstein has been asking “why” in neuroscience for years. She studied psychology with minors in neuroscience and medical anthropology at the University of North Carolina at Chapel Hill, then pursued a postbac at the National Institute of Environmental Health Sciences, part of the NIH. It was there that she joined a behavioral core lab, performing behavioral assays and pushing for answers to the “why” questions of psychology. Joining the IPN was a way to further explore the causational relationships between brain mechanisms and behavior.
Bernstein’s project is backed by the Neural Injury and Plasticity (NIP) T32 Training Program, within the university’s Center for Neural Injury and Recovery. From weekly journal clubs to workshops on ethics, rigor and reproducibility, she has found that the program opens new avenues for making a difference through research. With the foundation she has gained from both the IPN and the T32 program, Bernstein aims to continue helping those with the neurological disorders she studies.
“As someone who knows people with disorders such as Parkinson’s disease and Alzheimer’s, I think it’s really important to do this kind of research where not a lot of people are focusing on such a niche topic,” Bernstein said. “[People with neurological disorders] can’t stick up for themselves in this sort of manner, without the background, so I think it’s really important to keep pushing science forward in that way and speak out for others.”
Joos Berghausen: From the Bench to Business

Joos Berghausen
When Joos Berghausen started pursuing his Ph.D. in Pharmacology & Physiology at Georgetown, he wasn’t sure what he wanted to do after graduation. Receiving a T32 grant through the Pharmacological Sciences Training Program (PSTP) helped him explore his options and ultimately connected him with the organization where he plans to work once he has earned his degree.
Before coming to Georgetown in 2021, Berghausen earned his bachelor’s degree in pharmaceutical science from the University of Freiburg in Germany, then did postbaccalaureate research at the NIH. “I like that the FDA is here, the government is here, NIH is here,” he said. “I had no idea what I wanted to do afterwards, so being close to all of these organizations made me think it would be a good place to go to school.”
As a T32 grantee, Berghausen took an internship with Oxford BioDynamics, a United Kingdom-based company with a U.S. office located just outside of Washington, D.C., in Gaithersburg, Maryland. When he finished his internship, he continued working as a marketing consultant.
“I was always interested in marketing, business administration and product development,” he said. “I just did this internship and I liked it a lot.”
In his role as a researcher, Berghausen studies whether tumor progression can be inhibited by the interactions between small molecular ligands and the EAG1 potassium channel, which is overexpressed in many cancers. As a consultant, he assists the Oxford BioDynamics sales and marketing teams by writing web content and product summary statements, and identifying doctors who might be interested in their products.
“Mostly I make collateral that then our sales team can use, comparing our products to other products on the market,” Berghausen said. “The company is also in cancer research, so often I have to keep the sales team updated on the current literature.”
Berghausen’s doctoral work helped prepare him for his career as a consultant. “My research is very basic science but it helped me understand my side job area because I read papers all the time for my Ph.D., and that knowledge translated well,” he said.
The flexibility of the T32 program made it a valuable experience for Berghausen. “It helped me understand once I’m done with school how I can transition from basic science to the pharmaceutical industry,” he said. “It was a really helpful experience for me for sure.”
Meghan Bullard: Serving through Science

Meghan Bullard
Biomedical research is “a form of worship” for Meghan Bullard – a way to “unfold the mysteries of the universe” while also living her Christian values. When she is working with tissue samples or poring over data, the Biology Ph.D. student is answering the call to care for others.
Bullard is part of an NIH-funded effort to find new treatments for multiple sclerosis (MS), in hopes of providing relief to patients in the devastating later stages of the disease. Her work, in the lab of Provost’s Distinguished Associate Professor Jeffrey Huang, is supported by the Georgetown-Howard Universities Center for Clinical and Translational Science (GHUCCTS) TL1 Training Program in Translational Biomedical Science (TBS). Bullard said working with researchers from different disciplines in the TL1 program has yielded valuable insights into the scientific process, along with the technical aspects of disease and treatment.
“To see the different perspectives that people approach the same problem is really fascinating and really exciting,” she said. “The whole point of the TL1 program is to try to accelerate work from the preclinical bench research to treatment. And so, getting to see the different perspectives [of] people who are focused more on the clinical side of things, versus the preclinical benchwork side of things … has been really cool.”
Bullard started her biology studies as an undergrad at Furman University in South Carolina, where she got her first lab position studying neuroinflammation and “fell in love with research.” An interest in science policy drew her to Washington, D.C., and Georgetown for her doctoral studies, but ultimately, she chose to focus on bench research in Huang’s Laboratory of Immuno-Regeneration Research.
Huang encouraged her to apply for the TBS TL1 program to advance her research skills and her professional development. The program has connected Bullard with colleagues across research areas, helped her to practice grant writing, and funded travel to conferences to network beyond the Georgetown community.
The program is “just a really great environment,” Bullard said. “They’ve been really supportive of me and my work as well, and really helped elevate my critical thinking, my grant writing, my presentation skills – all of that, to the next level.”
Through all her work, Bullard finds inspiration in her faith.
“It actually has really driven my passion for science and my love of science,” she said. “I see my work as a form of worship, like getting to work alongside God to uncover and unfold the mysteries of the universe that until now, only He has known.”
Malak Mackie: Sharing Insights Across Disciplines

Malak Mackie
When Malak Mackie accepted her T32 grant, she knew it would go a long way toward funding her research. What she didn’t realize was that the grant would give her much more than money.
Pursuing a Ph.D. in Biochemistry and Molecular & Cellular Biology under the mentorship of Kathryn Sandberg and Aline de Souza since 2023, Mackie studies cardiovascular and renal impairment in late-term pregnancy – specifically, how these systems are impacted by periods of severe food restriction.
“The impact [of my research] is for any populations undergoing severe food restriction, voluntary or involuntary,” Mackie explained. “But also to treat predisposition to cardiovascular disease or chronic kidney disease – which is so important, because kidney transplant is number one in the world for fibrosis or acute or chronic kidney disease.”
Mackie uses female rats to model severe food restriction, refeeding, and pregnancy. She can then derive data such as protein expression in the kidney cortex during pregnancy, as well as sodium and potassium levels in urine.
For Mackie, this project is part of a long resume of biochemical and molecular research. After receiving her master’s in biotechnology and biodefense from American University, she went on to teach forensic chemistry lab as an adjunct there. In 2019, she began working at MedStar Georgetown University Hospital in a clinical laboratory – first in transfusion medicine, then as a medical laboratory scientist in molecular pathology and diagnostics (infectious disease division). Eventually, she realized “you can only grow so much in a clinical setting without a Ph.D. I [wanted] to get into a bench-to-bedside manner of clinical translational research, and to do that, you need your Ph.D.”

Mackie (second from right) poses with fellow members of the IMSD’s 2023 cohort.
Once Mackie was accepted into the Ph.D. program at Georgetown, she was also selected as her cohort’s fellow for the Initiative for Maximizing Student Development (IMSD), a two-year interdisciplinary T32 program focused on preparing scholars for careers in science. Mackie’s combined background in biotechnology and clinical labs made her an ideal candidate, but being in the IMSD program also paved the way for her to explore new opportunities: “There are so many events that come with IMSD, from the grant essentially. The first event I attended was the American Association for the Advancement of Science. That was fully funded through the grant through the IMSD, and I went with one of my IMSD peers. We got to go there together, we learned together, and we experienced the AAAS conference in a really exciting way.”
Two years later, Mackie is now presenting her own research at one of these events. She will be sharing data from two successful rat cohorts at the American Physiological Society Conference in late April, marking a significant milestone in her Ph.D journey.
Being an IMSD fellow has supported Mackie’s pursuit of clinical translational research, and in her eyes, that career could take so many forms. “If I could do clinical research at somewhere like the NIH, and teach, maybe here at Georgetown, that would be ideal – or if I could teach and also have my own lab, where I could take on students like myself, while continuing to do research.”
By Nikki Farnham, Natalie Rabner and Kat Zambon
